Evidence suggests that any patient undergoing surgery for more than three hours faces a risk of developing pressure sores – decubitis ulcers – caused by immobility during the procedure and the use of anaesthesia. As well as causing pain, this obviously increases the risk of infection – which in turn can mean longer stays in hospital with all the associated costs to already stretched NHS budgets.
As NHS staff work hard to reduce the waiting lists for hospital treatment (which in March 2023 stood at a record high of over 7.3 million) – there is a renewed focus on reducing these ‘Hospital-Acquired Pressure Injuries (HAPIs).’
Background
The UK’s experts in evidence-based best practice and value for money, the National Institute for Health and Care Excellence (NICE), say pressure ulcers represent a major burden of sickness and reduced quality of life for people with pressure ulcers – and their carers¹.
In 2018, it was estimated that the daily cost to the NHS to treat pressure related injuries was a staggering £3.8 million². And then there is litigation – which cost the NHS a further £20.8 million for cases involving pressure ulcers in 2017-18 – a figure representing an increase of 53% in three years³.
So what can be done? The NHS Improvement paper Pressure ulcers: revised definition and measurement describes these injuries as ‘concerning, and mainly avoidable harm, associated with healthcare delivery’⁴ which focuses attention firmly on prevention rather than cure and, in the operating theatre, this involves both high level tissue viability practices and specially designed positioning products.
What causes pressure ulcers?
A decubitis ulcer, or pressure sore, is an injury to the skin caused by constant pressure resulting from impaired mobility.
The pressure of the patient’s body weight reduces blood flow – particularly to bony extremities – eventually causing cell death, skin breakdown, and the development of an open wound.
The stages are determined as:
STAGE 1
Skin may appear reddened, like a bruise. The integrity of the skin remains intact – there are no breaks or tears, but the area is at high risk of further breakdown. It is crucial that the risk is identified promptly, as, with effective treatment, this level of damage will heal within 60 days.
STAGE 2
Skin breaks open, wears away, and forms an open sore or ‘ulcer’.
STAGE 3
The sore worsens and extends beneath the skin surface, forming a small crater. There may be no pain at this stage due to nerve damage. The risks of tissue death and infection are high.
STAGE 4
Condition becomes more severe with extensive damage to deeper tissues (muscles, tendons, and bones). Serious complications, such as osteomyelitis (infection of the bone) or sepsis (infection carried through the blood) can occur⁵.
Contributory factors
There are many contributory factors (some of which may be interlinked) that can make a patient more susceptible to pressure ulcers.
These include:
AGE - Both ends of the age spectrum: children, especially neonates, and the elderly have less resilient skin, and in the latter, both dementia and lack of mobility can be exacerbating factors.
BUILD - Those who are overweight or obese carry the concern about conditions such as diabetes (see ‘Underlying health conditions’ below) while those underweight may have less tissue (muscle mass), more bony prominences and thinner skin.
BROKEN OR FRAGILE SKIN - Perhaps due to conditions such as Eczema or Psoriasis or simply age, this can make a patient more vulnerable.
NUTRITION - A good diet is necessary for healthy skin, so under or poorly nourished or hydrated patients are at greater risk.
MOISTURE (CONTINENCE / PERSPIRATION / WOUND EXUDATE) - Moisture under pressure against the skin can create moisture legions which can eventually lead to ulceration⁶⁻⁷.
MOBILITY - Already sedentary or immobile patients present a greater risk, which is compounded by the complete immobility of general anaesthesia.
MEDICATION - Drug-induced pressure ulcer (DIPU) is a newly recognised adverse drug reaction associated with the administration of psychiatric drugs in geriatric patients with dementia.
UNDERLYING HEALTH CONDITIONS - Conditions that affect the flow of blood through the body, such as type 2 diabetes, can make a patient more vulnerable to pressure ulcers. Can also be a concern with some heart, lung and kidney illness⁸.
MEDICAL DEVICE-RELATED PRESSURE INJURIES - Any piece of medical equipment in contact with the patient over an extended period has the potential to cause a pressure injury, even something seemingly innocuous such as an intubation tube resting against a patient’s face. Achieving adequate support and ensuring the patient remains rigidly in the desired position during surgery, means care must be taken in selecting appropriate positioning devices.
While many of these factors are intrinsic to individual patients, the final one offers the greatest scope for prevention.
Areas of greatest vulnerability
As stated earlier, pressure injuries commonly develop in the areas of the body in contact with a surface:
Back of head and ears
Lower back and buttocks
Inner knee
Shoulder
Greater trochanter / Hip
Heel
Elbow
N.B. Pressure injuries may also form in places where the skin folds over itself and can also occur where medical equipment puts pressure on the skin, e.g. they may form where oxygen tubing presses on the ears or cheeks⁹.
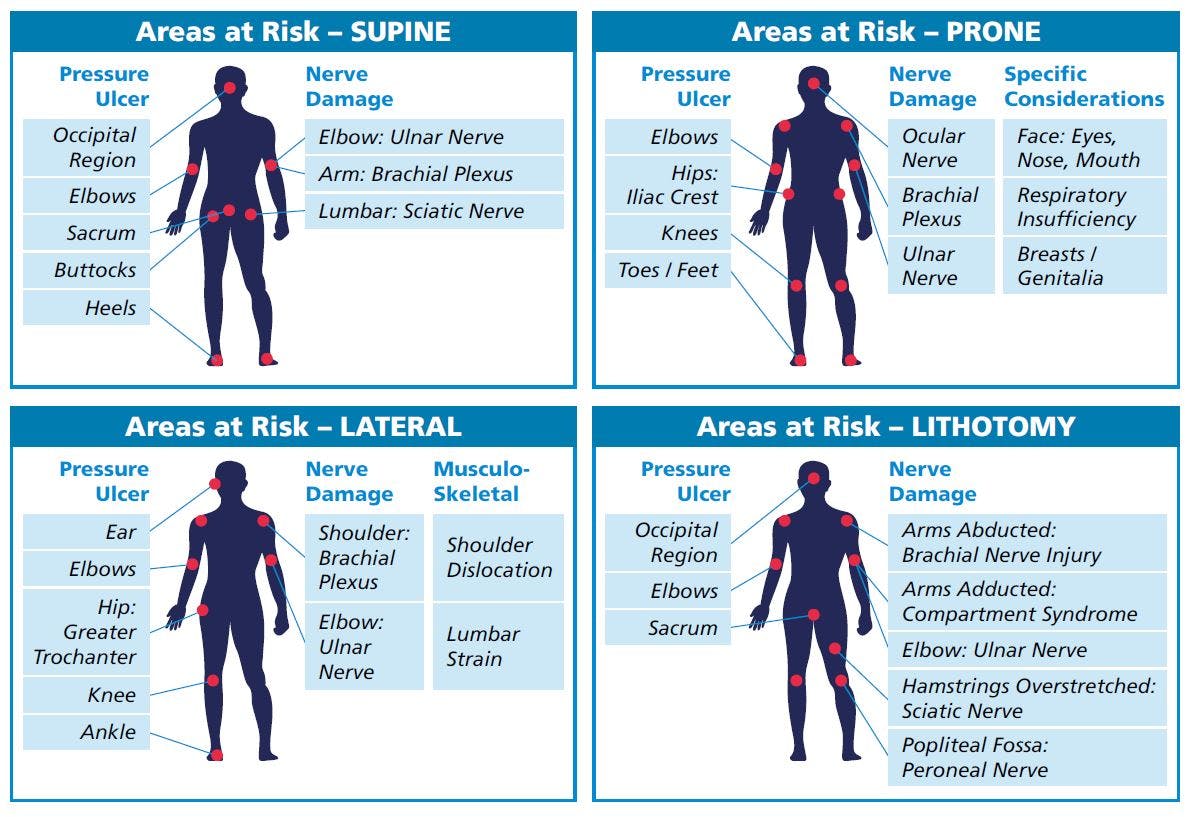
The combination of these will vary depending on the patient's position during surgery, as follows:
Recent research has also shown the likely incidence of pressure sores according to hospital department¹⁰
An additional complication - Surgically-induced Neuropathic Pain
Pressure injuries during surgery are not only linked to postoperative pressure ulcers, but also to Surgically-induced NeuroPathic Pain (SNPP)¹¹.
This is caused because the peripheral nervous system links the central nervous system to every other part of the body and when a peripheral nerve is damaged during surgery, proper communication between the brain and the body is interrupted – resulting in loss of sensation, muscle weakness and pain. It is a nerve injury which a significant number of patients (10 to 40%) experience.
The initiating surgery and nerve damage set off a cascade of events that include both pain and an inflammatory response, resulting in ‘peripheral’ and ‘central sensitisation’, with the latter resulting from repeated barrages of neural activity from nociceptors. In affected patients these initial events produce chemical, structural and functional changes in the peripheral (PNS) and central nervous (CNS) systems. The maladaptive changes in damaged nerves lead to peripheral manifestations of the neuropathic state – allodynia, sensory loss, shooting pains etc., that can manifest long after the effects of the surgical injury have resolved.
Surgical positioning is the key to minimising this risk.
Implications for Clinical Practice
In 2015, NICE published Quality Standard [QS89] covering the prevention, assessment and management of pressure ulcers in all settings, including hospitals¹².
This has implications for the clinical practice within the operating room and states that:
Operating departments should have clinical guidelines covering the prevention of pressure injuries
Perioperative practitioners should play a pivotal role in ensuring the patient receives adequate pressure injury protection and act as the patient advocate during surgery
The operating room team should be fully briefed on the pressure care needs of the patient
Each operating room should be adequately equipped with a full range of suitable pressure redistributing devices
Perioperative practitioners should be adequately trained in pressure injury prevention and the use of pressure redistributing devices.
The guidelines stress taking patient contributory factors (as noted earlier) into consideration along with other aspects including the age profile of the patient for the type of surgery involved, the surgical position required for the procedure and its likely duration. Appropriateness of operative repositioning and the availability of a tissue viability practitioner might also offer opportunities to mitigate the risks of pressure ulcers developing.
Preventative Measures
Most crucially, an earlier published set of NICE guidelines (Pressure ulcers: prevention and management clinical guideline [CG179] Published: 23 April 2014) focus on preventative measures¹³.
Aimed at all healthcare professionals, its recommendations include comprehensive advice on all patients from neonates to adults including:
Risk assessment
Skin assessment
Repositioning
Skin massage
Nutritional supplements and hydration
Pressure redistributing devices
Barrier creams
Care planning
Patient and carer information
Those particularly relevant to the operating theatre include:
RISK ASSESSMENT – clearly a vital first step as, regardless of the patient-related contributory factors, all patients have the potential to develop a pressure related injury. It is more likely to occur in patients who have a serious underlying medical condition, a neurological condition, impaired mobility, impaired nutrition, poor posture or a deformity, but the approach to every patient should be the same to mitigate the risks. The recommendations are therefore:
Adults:
- Be aware that all patients are potentially at risk of developing a pressure ulcer
- Carry out and document an assessment of pressure ulcer risk for adults
- Consider using a validated scale to support clinical judgement (for example, the Braden scale, the Waterlow score or the Norton risk-assessment scale)
- Reassess pressure ulcer risk if there is a change in clinical status.Neonates, infants, children and young people:
- Carry out and document an assessment of pressure ulcer risk for neonates, infants, children and young people
- Use a scale validated for this population (for example, the Braden Q scale for children).
POSITIONING THE PATIENT FOR SURGERY – critical in the prevention of pressure ulcers and surgically induced neuropathic pain. The introduction of pressure, friction and shear forces when positioning the patient for surgery can be a major contributing factor in the outcome for the patient postoperatively.
OPERATIVE REPOSITIONING OF THE PATIENT – it is generally accepted that repositioning people who are at risk of developing a pressure ulcer can prevent one developing by removing pressure from the at-risk site.
IDENTIFYING THE MOST EFFECTIVE POSITION – and the optimum frequency of repositioning – will minimise discomfort and maximise pressure ulcer prevention.
The frequency of repositioning during surgery can only be a clinical decision made locally; NICE guidance states this should be at least every four hours, but good practice amongst pressure care professionals calls for at least every two.
PRESSURE REDISTRIBUTING DEVICES – as detailed in the NICE guidelines, operating departments should consider the use of pressure redistributing devices for all patients during surgery.
Pressure redistribution devices work by reducing or redistributing pressure, friction or shear forces.
Devices include high‑specification mattresses, pressure redistribution cushions and equipment that offloads heel pressure.
The type of device a person needs will depend on their circumstances, for example, their mobility, the results of the skin assessment, their level of risk, the site that is at risk, the person’s weight and the person’s general health.
Using pressure redistribution devices as soon as possible can prevent pressure ulcers developing and help to treat them if they do arise, ensuring patient safety and improving the experience of people at high risk of pressure ulcers.
An in-depth review of pressure redistributing devices is included below.
Pressure redistributing devices
OPERATING TABLE MATTRESS
Operating table manufacturers supply their devices with mattresses which, in the modern era, are generally adequate in providing basic pressure relieving properties and are described as ‘Continuous Low Pressure (CLP)’ support surfaces.
Defined as ‘low-tech’ or ‘non-powered’, these surfaces consist of a core of material, or combination of materials, plus a breathable cover, but they are ‘passive’, in other words, there is no powered ripple / undulating movement to counteract the effects of the patient’s immobility.
While these devices are grouped together as a category – their effectiveness varies greatly depending on their composition and construction.
The two main types of CLP devices found in healthcare facilities are:
STANDARD FOAM MATTRESS (SFM)
An SFM is generally regarded as a support surface produced using a single piece of plain cut, low density / low hardness grade, open cell foam.
It will offer pressure care suited to patients who weigh circa 180kg and present a low to medium pressure care risk.ALTERNATIVE FOAM MATTRESS (AFM)
An alternative foam mattress (AFM) is generally regarded as a support surface produced using a combination of foam specifications which may vary in density, hardness and construction (the so called ‘cutting methods’). The foam may be elastic or viscoelastic, open or closed cell, or a combination of these.
It will offer pressure care suited to patients who weigh circa 250kg and present a medium to high pressure care risk.
For further information see our paper ‘Pressure redistributing surfaces: getting to the core of the subject¹⁴.’
However, a CLP support surface cannot be adopted as a universal solution, as this will not mitigate all of the risks associated with the contributory factors that may be encountered, especially for extended surgical procedures or certain surgical positions where an isolated proportion of the patient’s anatomy is bearing their weight during surgery.
POSITIONING DEVICES
To achieve adequate support and ensure the patient remains rigidly in the desired position during surgery, means that some positioning devices are supplied with a high hardness pad. An unintended consequence of this may be its contribution to a postoperative pressure injury. This can however be mitigated by the addition of products specifically designed to redistribute pressure away from particular parts of the body.
PRESSURE REDISTRIBUTING CUSHIONS
A series of additional pressure redistributing cushions can be employed, either as single-use uncovered foam, or reusable material covered foam. These will generally be designed and manufactured to suit a particular element of patient anatomy or a specific surgical position.
While these may offer some alleviation in pressure, they are, in the main manufactured from the same foam as either an SFM or AFM mattress (detailed earlier in this document) and may not prove to be as effective as alternative solutions that are available.
These are also costs associated with the disposal of single-use medical devices for healthcare facilities – to say nothing of the environmental impact.SILICONE GEL PRESSURE REDISTRIBUTING CUSHIONS (PRCs)
It is generally accepted that a pressure redistributing device should have the ability to reduce capillary interface pressures to 32mmHg or less.
One of the most effective and reliable solutions available is medical grade silicone, which has been employed within operating theatre departments in the UK since 1995.
Globally, similar devices have been available since the mid-1980s, in the form of ultra-soft synthetic rubber polymer.
Medical grade silicone is a viscoelastic material that is as soft as skin and mimics underlying fatty tissue, redistributing pressure in an extremely effective manner whilst dampening and absorbing impact in combination with reducing shear forces and friction.
As an example: a scapula without the protection of a silicone gel PRC may experience pressure of circa 64mmHg, and that will reduce to 9mmHg when one is used.
It is also hypoallergenic, latex free, x-ray translucent, MRI compatible, non-conductive, antimicrobial, thermally stable (can be cooled or heated) and enduring.
Silicone gel PRCs are designed and manufactured in a way that allows them to accommodate a patient’s anatomy, alleviating pressure and protecting it in the key areas – whilst also offering optimal patient positioning for surgery.
The design of many of these devices allows versatility, so they can be employed in combination with other positioning devices or in between overlaid parts of a patient’s anatomy (e.g. between knees in the lateral position).
Whilst the use of silicone gel PRCs cannot be a 100% mitigation of risk from a pressure injury – in lieu of every patient being pressure mapped during a procedure – it has proven itself to be a highly reliable method of protection to date.
Summary
The cost of pressure injuries in terms of patient pain and discomfort cannot be measured, but the cost of treating them can, and within the constrained budgets of the NHS, it is clear that products which can help to prevent pressure sores occurring in the first place must be cost effective, durable and easy to use. Silicone pressure redistributing cushions address all of these factors and can play a major role in preventative measures within an operating department.
You can download our interactive positioning paper here.
For further information, you can contact our team by clicking the link here.
References
https://www.nice.org.uk/guidance/cg179/documents/pressure-ulcers-scope2
https://www.england.nhs.uk/wp-content/uploads/2021/09/NSTPP-summary-recommendations.pdf
https://www.nursingtimes.net/news/technology/nhs-litigation-bill-for-pressure-ulcers-soars-53-in-three-years-08-05-2019/
NSTPP-summary-recommendations.pdf (england.nhs.uk)
https://jamanetwork.com/journals/jama/fullarticle/203224
Causes and strategies for moisture lesions | Nursing Times
NU-18-Moisture-Damage-Pressure-Ulcer-Prevention-v5-web.pdf (jpaget.nhs.uk)
Pressure ulcers – Illnesses & conditions | NHS inform
https://myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=zm2441
The Incidence of Pressure Ulcers and its Associations in Different Wards of the Hospital: A Systematic Review and Meta-Analysis – PMC (nih.gov)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3546123/
https://www.nice.org.uk/guidance/qs89/chapter/Introduction
https://www.nice.org.uk/guidance/cg179
https://anetic-aid-production-assets.s3.eu-west-1.amazonaws.com/Articles/pressure-redistributing-surfaces.pdf


